Advanced Clinical Services for Optimal Eye Health and Visual Well-being

Cataract

Glaucoma

Diabetic Retinopathy

Retinal Diseases & Vitrectomy

Age-Related Macular Degeneration

Cornea And External Eye Diseases
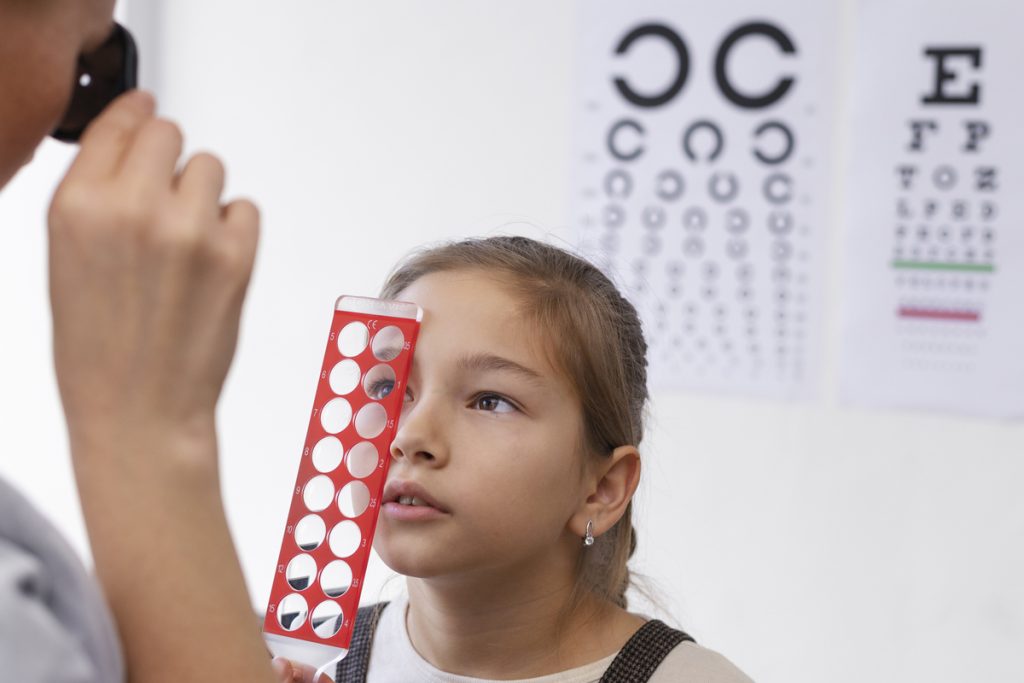
Children’s Eye Disorders

Retinal Detachment

Contact Lenses & Glasses

Cataract

Glaucoma

Diabetic Retinopathy

Retinal Diseases & Vitrectomy

Age-Related Macular Degeneration

Cornea And External Eye Diseases
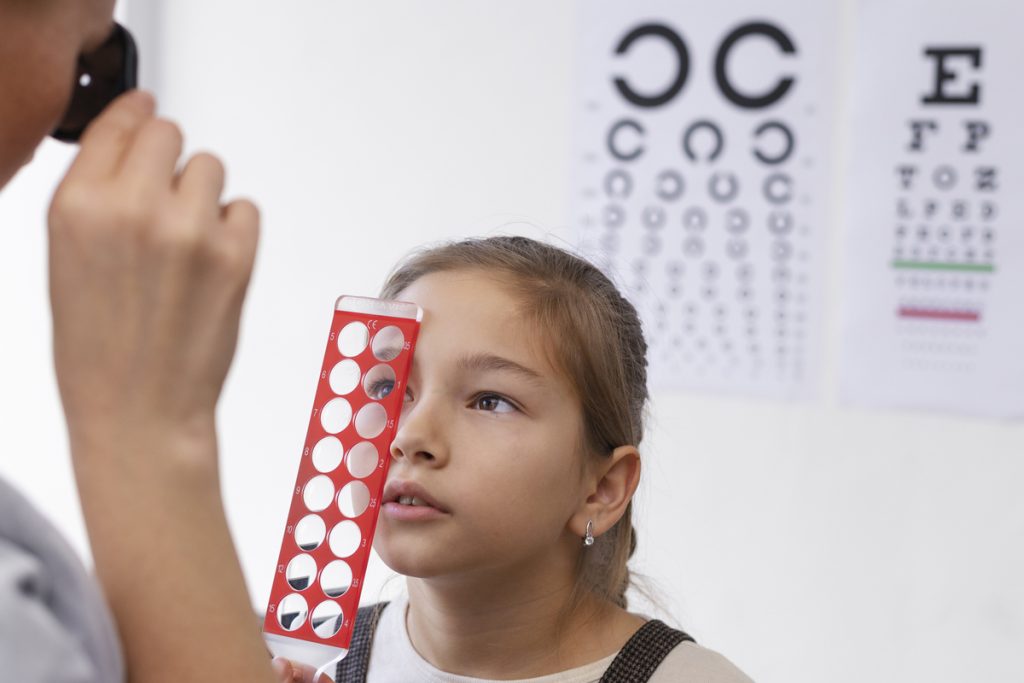
Children’s Eye Disorders

Retinal Detachment

